Hematophagous organisms, like ticks, leeches, mosquitoes, and nematodes, use a quick-acting mechanism to prevent clotting while acquiring blood meals from a host. A team of scientists has harnessed the secret behind this strategy as a potential anti-clogging agent.
Mimicking Anti-Clotting Agent
At Duke University Medical Center, experts described a synthetic molecule that can mimic the features of compounds present in the saliva of blood-sucking organisms. The findings of the study were published in the paper "Aptameric hirudins as selective and reversible EXosite-ACTive site (EXACT) inhibitors."
According to senior author Bruce Sullenger, biology and evolution have figured out anticoagulation several times with a highly potent strategy. The research team observed that all blood-sucking organisms have evolved a similar system to prevent blood clotting. Their saliva contains an anti-clotting agent, which uses a two-pronged process.
First, the agent binds to the surface of clotting proteins in the host's blood. Next, it enters the protein's core to temporarily inactivate clotting during a blood meal.
Blood-suckers target various proteins among the over two dozen molecules involved in blood clotting. In this study, the research team focused on engineering molecules to concentrate on thrombin and factor Xa in human blood. Led by Haixiang Yu, the team successfully achieved dual-action anti-clotting activities against these proteins.
The next challenge was finding a way to reverse the process. This concern has important clinical applications, as it ensures that patients do not suffer from hemorrhage. Using a fully elucidated activation mechanism, the scientists reverse-engineered an antidote that restores clotting quickly.
Another important feature of the new agent is that it is a synthetic molecule that functions differently from heparin, isolated from pig intestines. Although it has been the clinical standard for the past century, heparin requires a massive farming infrastructure, which generates greenhouse gases and air pollution.
How Does Blood Clot?
When a blood vessel is damaged, the injured cells in the vessel wall release chemical signals that cause clots, which slow or stop bleeding. A blood clot is formed through several steps.
First, the chemical signals released by the damaged cells travel through the bloodstream to the spleen, where most of the platelets are stored. The chemical signals tell the spleen to release the platelets into the blood. At the injury site, the vessel walls become sticky and capture the released platelets as they float past.
The platelets then change their shape and become stickier. This enables them to attach to the vessel wall and clump together to form a platelet plug.
Normally, the clotting factors are turned off so that an individual does not form abnormal blood clots. During an injury, platelets release molecules into the bloodstream that help turn no clotting factors.
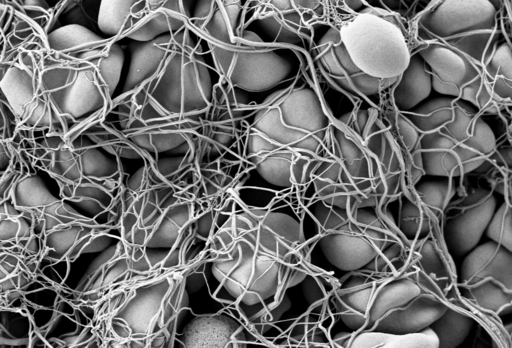
One vital clotting factor is fibrin, which, when turned on, forms a mesh to keep the platelet plug in place. The mesh traps the red blood cells to form a blood clot. The platelets also contract to pull the two sides of the damaged blood vessel closer together, making them easier to repair.
RELATED ARTICLE : Nanocapsules on Blood Clot Drugs Reduce Side Effects, Increase Efficacy
Check out more news and information on Blood Clot in Science Times.
© 2025 ScienceTimes.com All rights reserved. Do not reproduce without permission. The window to the world of Science Times.











