This article will provide a scientific explanation and description of sleep apnea, what kind of disease it is, and which categories of people are most often susceptible to it. Also, how this type of disease occurs and affects a person's life. Statistics on morbidity will be analyzed. Recommendations will be given on how to treat and what to use in a situation where similar symptoms are found in a person.
Sleep apnea is a sleep disorder where breathing stops and starts continually during sleep. There are three main types of sleep apnea:
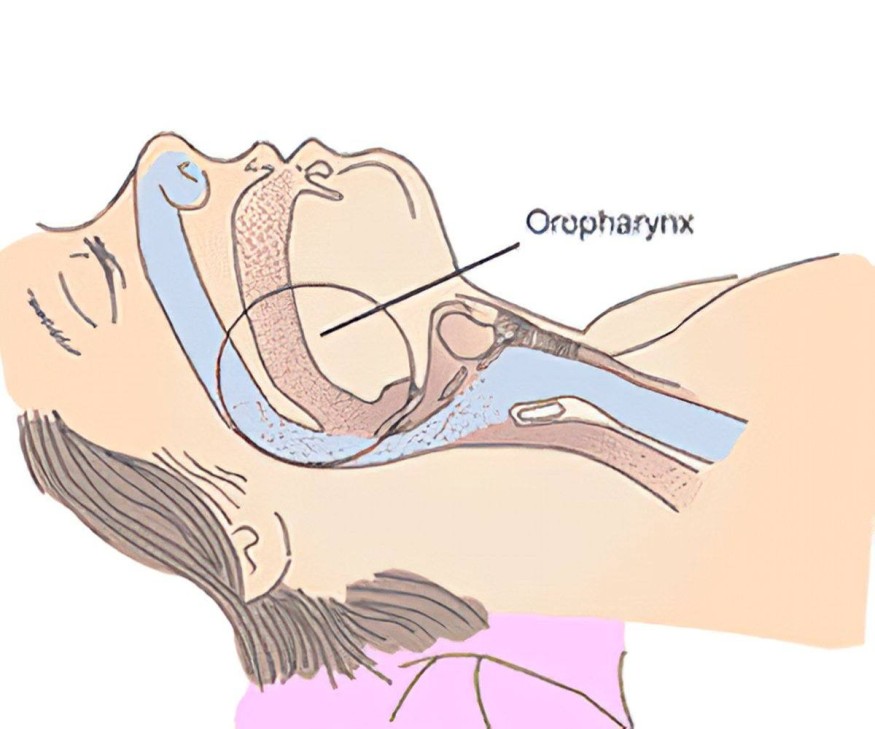
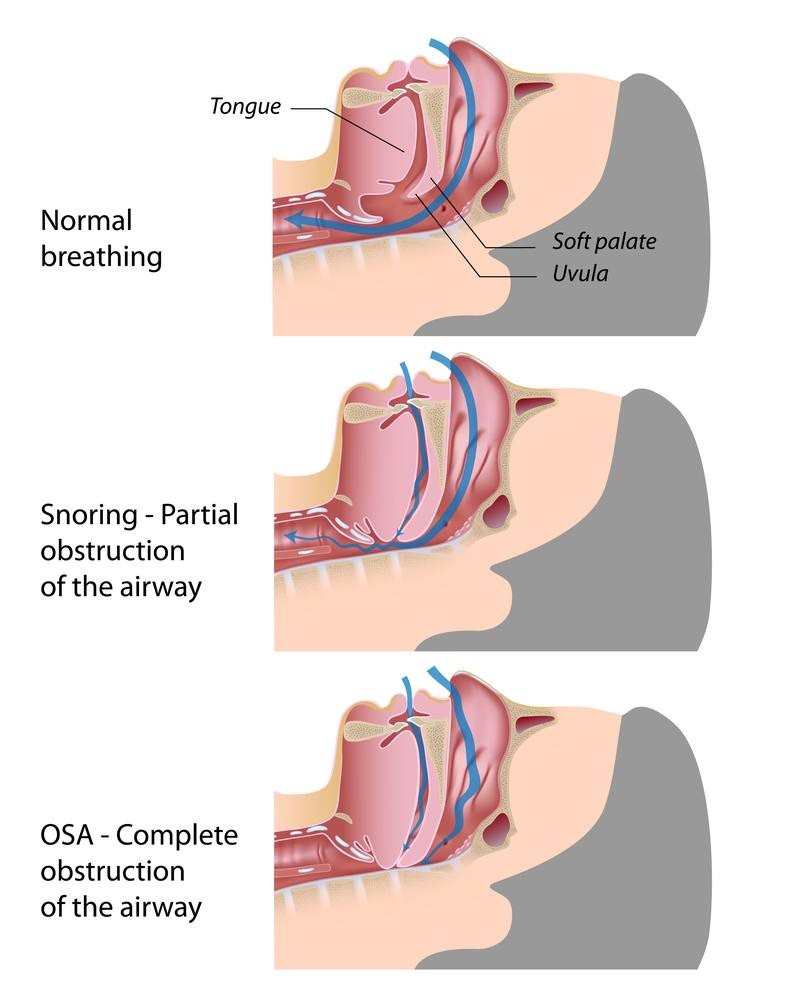
Obstructive Sleep Apnea (OSA): This is the most common type, where the muscles in the throat relax excessively, causing airway blockage.
Central Sleep Apnea (CSA): In this type, the brain fails to send the proper signals to the muscles that control breathing. It's less common than OSA.
Complex Sleep Apnea Syndrome (also known as Mixed Sleep Apnea): A combination of obstructive and central sleep apnea. It typically starts as OSA and evolves into CSA using continuous positive airway pressure (CPAP) therapy.
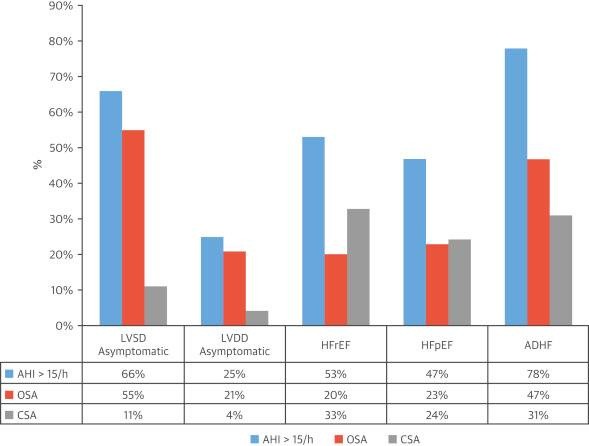
Sleep apnea has severity levels that are categorized based on the frequency of breathing disruptions. Also known as the Apnea-Hypopnea Index (AHI):
Mild: AHI score of 5 to 15 events per hour. It means there are 5 to 15 instances of complete breathing-stopping (apneas) or significant reductions in airflow (hypopneas) per hour of sleep.
Moderate: AHI score of 15 to 30 events per hour. It indicates a higher frequency of apneas and hypopneas during sleep.
Severe: AHI score of more than 30 events per hour. It means there are frequent and severe disruptions in breathing during sleep. It's important to note that the AHI score is just one aspect considered when diagnosing and assessing sleep apnea.
Several risk factors can increase the likelihood of developing sleep apnea. Some of these include:
Excess Weight: Obesity is a significant risk factor, as it can accumulate fat around the upper airway, obstructing breathing during sleep.
Neck Circumference: People with a thicker neck may have a narrower airway, increasing the risk of airway obstruction.
Age: Sleep apnea is more common in middle-aged and older adults, although it can affect people of all ages.
Gender: Men are more likely than women to develop sleep apnea, though the risk for women increases if they are overweight, and it also becomes more common after menopause.
Family History: A family history of sleep apnea or other sleep disorders may increase your risk.
Smoking and Alcohol Use: Both smoking and excessive alcohol consumption can increase muscle relaxation in the throat, leading to airway obstruction.
Nasal Congestion: If you have difficulty breathing through your nose due to allergies, sinus issues, or anatomical factors, you are at a higher risk of sleep apnea.
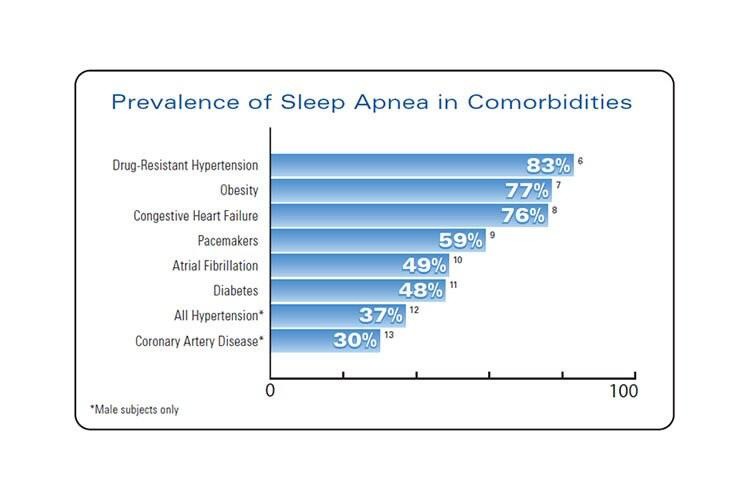
Medical Conditions: Conditions of high blood pressure, heart disorders, type 2 diabetes, and hormonal disorders can increase the risk of sleep apnea.
Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, and Pacific Islanders, have a higher prevalence of sleep apnea.
Use of Sedatives: Sedatives, tranquilizers, and sleeping pills can relax the muscles in the throat, potentially increasing the risk of airway obstruction.
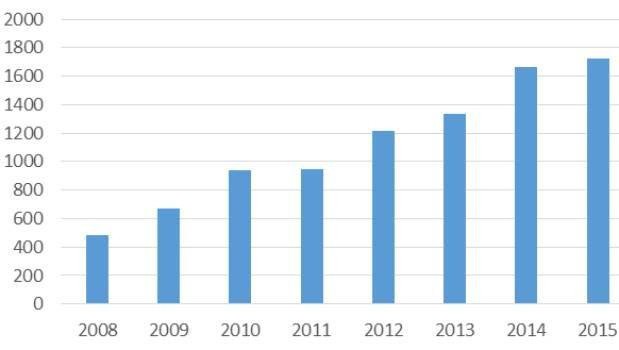
Studies suggest that the risk for sleep apnea increases with age. The American Journal of Respiratory and Critical Care Medicine has estimated that over 22% of all adults, ages 18-90, have Obstructive Sleep Apnea alone. According to the American Medical Association, it is believed that more than 30 million people have sleep apnea in the US, about 9% of the population. The majority of these cases are thought to be caused by Obstructive Sleep Apnea.
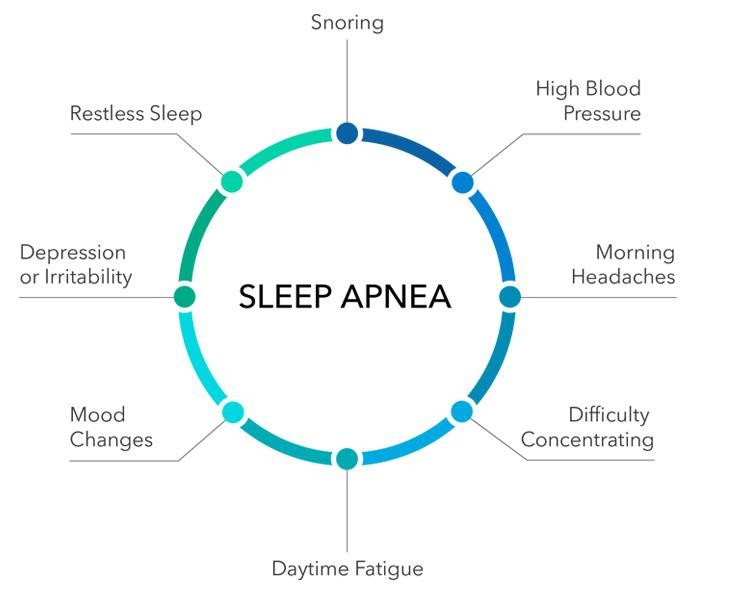
Sleep apnea can have various significant impacts on both your physical health and overall well-being:
Daytime Fatigue: The repeated disruptions in sleep caused by sleep apnea can lead to excessive daytime sleepiness, which in turn can affect your ability to concentrate, work, drive safely, and perform daily tasks.
Cardiovascular Health: Sleep apnea is associated with an increased risk of high blood pressure, heart disease, stroke, and irregular heartbeats (arrhythmias). The interruptions in breathing can strain the cardiovascular system.
Metabolic Health: Sleep apnea has been linked to insulin resistance and type 2 diabetes. Poor sleep quality and disruptions in sleep patterns can affect glucose metabolism.
Weight Gain: Sleep apnea and weight gain often have a bidirectional relationship. Excess weight can contribute to sleep apnea, and sleep apnea can lead to weight gain due to disruptions in metabolism and hormonal changes.
Mood Disorders: Sleep apnea can contribute to or exacerbate mood disorders such as depression and anxiety. The disrupted sleep patterns and oxygen deprivation during sleep can impact mood regulation.
Cognitive Impairment: Cognitive functions such as memory, concentration, and decision-making can be impaired due to inadequate sleep caused by sleep apnea.
Decreased Quality of Life: The constant fatigue and health issues associated with sleep apnea can lead to a decreased overall quality of life.
Relationship Strain: Loud snoring and frequent awakenings due to sleep apnea can disrupt your bed partner's sleep, leading to relationship strain and fatigue for both individuals.
Increased Risk of Accidents: The daytime sleepiness caused by sleep apnea can increase the risk of accidents while driving, operating machinery, or performing other activities that require attention.
Worsening of Other Medical Conditions: Sleep apnea can worsen existing health conditions, such as asthma, chronic obstructive pulmonary disease (COPD), and chronic pain.
Surgery and Anesthesia Complications: If you have sleep apnea and require surgery, you may be at a higher risk for complications related to anesthesia and the effects of interrupted breathing during the procedure.
The treatment for sleep apnea depends on the severity of the condition and the specific type of sleep apnea. Here are some common treatment options:
1. Lifestyle Changes:
- Weight Loss: If you're overweight, losing weight can often help reduce the severity of sleep apnea.
- Positional Therapy: Some people experience more pronounced apnea when sleeping on their backs. Sleeping on your side might alleviate the symptoms.
2. Medical intervention:
Continuous Positive Airway Pressure (CPAP): This is one of the most effective treatments for obstructive sleep apnea. A CPAP machine delivers a constant stream of air through a mask to keep your airway open during sleep.
Bi-level Positive Airway Pressure (BiPAP): Similar to CPAP, a BiPAP machine delivers varying levels of pressure when you breathe in and out. It's often used for more severe cases of sleep apnea or for individuals who have difficulty tolerating CPAP.
Oral Appliances: These are devices that can be worn in the mouth to reposition the lower jaw and tongue, helping to keep the airway open.
Adaptive Servo-Ventilation (ASV): This treatment is used for complex sleep apnea. ASV devices monitor your breathing patterns and adjust pressure to stabilize your breathing.
Expiratory Positive Airway Pressure (EPAP): These are small, disposable devices that you place over your nostrils before sleeping. They create resistance during exhalation to help keep the airway open.
3. Surgery:
- Uvulopalatopharyngoplasty (UPPP): This surgery involves removing excess tissue from the throat to widen the airway.
- Genioglossus Advancement (GA): The tongue muscle attachment is repositioned to prevent airway collapse.
- Maxillomandibular Advancement (MMA): The upper and lower jaw are moved forward to enlarge the airway.
Reference list and bibliography:
1) https://pubmed.ncbi.nlm.nih.gov/34904935/
2) Lavie P. Restless Nights: Understanding Snoring and Sleep Apnea. Yale University Press; 2008
3) Gottlieb DJ, Punjabi NM. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA. 2020 Apr 14;323(14):1389-1400. [PubMed]
4) Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991 Dec;14(6):540-5. [PubMed]
5) Learmonth YC, Dlugonski D, Pilutti LA, Sandroff BM, Klaren R, Motl RW. Psychometric properties of the Fatigue Severity Scale and the Modified Fatigue Impact Scale. J Neurol Sci. 2013 Aug 15;331(1-2):102-7. https://pubmed.ncbi.nlm.nih.gov/23791482
6) Coniglio AC, Mentz RJ. Sleepbreathing disorders in heart failure. Heart Fail Clin. 2020; 16:45-51. doi: 10.1016/j.hfc.2019.08.009
7) Coniglio AC, Mentz RJ. Sleepbreathing disorders in heart failure. Heart Fail Clin. 2020; 16:45-51. doi: 10.1016/j.hfc.2019.08.009
© 2025 ScienceTimes.com All rights reserved. Do not reproduce without permission. The window to the world of Science Times.











