Scientists at the University of Southern California have developed a "heart attack on a chip" microscale model that can replicate key aspects of myocardial infarction. This device has the potential to serve as a testbed for developing new heart drugs and personalized medicines in the future. USC researchers Megan McCain and postdoc Megan Rexius-Hall engineered the "heart attack on a chip" at the University of Southern California's Alfred E. Mann Department of Biomedical Engineering.
The device, developed by the researchers, can be used to clearly understand how the heart is changing after a heart attack, allowing for the development and testing of drugs that can limit the further degradation of heart tissue that can occur after a heart attack.
The microscale model can replicate some key features of a heart attack in a simple and easy-to-use system. Megan McCain, a cardiac tissue engineer whose work includes co-developing a heart on a chip, and Rexius-Hall have published their findings in the journal Science Advances in an article titled "A Myocardial Infarct Border-Zone-On-A-Chip Demonstrates Distinct Regulation of Cardiac Tissue Function by an Oxygen Gradient."
America's Worst Enemy
Coronary heart disease is the leading cause of death in the United States, with 360,900 Americans succumbing to it in 2018. This accounted for 12.6% of all deaths in the country, according to the American Heart Association. A heart attack, which is a severe form of coronary heart disease, occurs when fat, cholesterol, and other substances in the coronary arteries greatly reduce the flow of oxygen-rich blood to part of the heart. Between 2005 and 2014, an average of 805,000 Americans had heart attacks each year.
Even if a patient survives a heart attack, they can still experience long-term effects such as fatigue, weakness, illness, and in some cases, death due to heart failure. This is because heart cells do not regenerate like other muscle cells; instead, immune cells appear at the site of injury, which can be harmful. Additionally, scarring develops which weakens the heart and reduces its ability to pump blood.
Researchers at the University of Southern California have developed a "heart attack on a chip" microscale model that can replicate key aspects of myocardial infarction. This device has the potential to serve as a testbed for developing new heart drugs and personalized medicines in the future. However, scientists do not fully understand the process of how heart cells in the healthy and injured parts of the heart communicate with each other and change after a heart attack.
McCain and Rexius-Hall believe that their heart attack on a chip can help to shed some light on these mysteries. Ultimately, the team wants to have a model that can lead to a better understanding of heart attack injury, said Rexius-Hall.
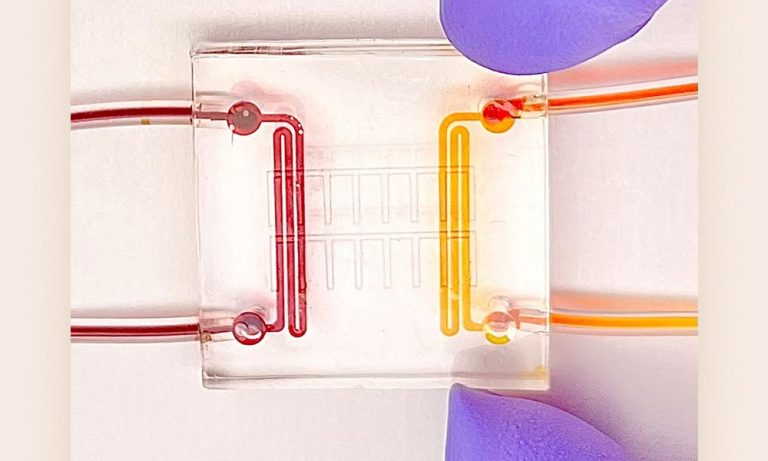
The heart attack on a chip is a microfluidic device that allows researchers to study heart attacks in real-time. The device is made of a rubber-like polymer called PDMS and is slightly larger than a quarter. It has two channels through which gasses flow and a thin layer of the same material that is permeable to oxygen. A layer of protein is patterned on top of the chip, and heart cells are grown on the protein. The device allows researchers to mimic a heart attack by exposing the heart cells to a gradient of oxygen.
ALSO READ : Genes Potentially Responsible for Coronary Heart Disease Triggers Cardiovascular Occurrences
Developing the Replication
The heart attack on a chip is composed of several layers. Above the base microfluidic device, a thin layer of the same rubber material is added. This layer is permeable to oxygen, allowing it to reach the heart cells. A layer of protein is then patterned on top of the chip, allowing the heart cells to align and form the same structure as a real heart. Finally, rodent heart cells are grown on top of the protein layer.
As explained by the researchers, to mimic a heart attack, gas with and without oxygen is released through the channels of the microfluidic device. This creates an oxygen gradient that simulates the conditions of a heart attack. By exposing the heart cells to this gradient, researchers can study the functional changes that occur in the heart during an attack, such as arrhythmia and contractile dysfunction. They can observe functional changes that occur in the heart after an attack, such as arrhythmia and contractile dysfunction.
This also permits the researchers to examine heart tissue in real-time. The device is small, clear, and easy to see under a microscope, which makes it ideal for observing functional changes in the heart after a heart attack. These changes can include arrhythmias (irregular heartbeats) and contractile dysfunction (decreased contraction strength of the heart). In the future, the model can be made more complex by adding immune cells or fibroblasts, the cells that generate scar tissue after a heart attack.
By contrast, traditional animal models and cell culture models do not allow researchers to observe changes in heart tissue. Additionally, traditional cell culture models expose heart cells to uniform levels of oxygen, but not a gradient, which means they cannot mimic the conditions that damaged heart cells experience in the border zone after a heart attack. The researchers behind the microfluidic device are excited about its potential to improve patient care and treatment for heart attacks.
RELATED ARTICLE: Doctors Can Use Selfies To Detect Cardiovascular Diseases
Check out more news and information on Heart Health in Science Times.











